Content warning: this article contains references to suicide and self-harm.
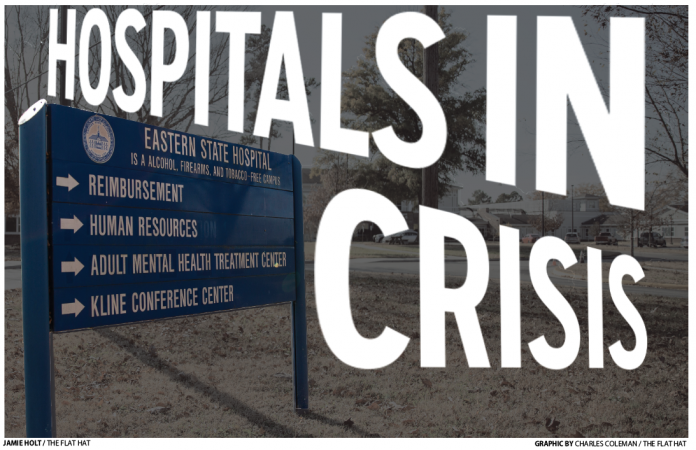
Friday, July 9, 2021, the Virginia Department of Behavioral Health and Developmental Services, DBHDS, announced bed reductions at five of the state’s public mental health facilities, including Eastern State Hospital in Williamsburg. In the months since, not much has changed for the strained, underfunded hospital. Likewise, support for supplementary, community-based mental health care is lacking.
Eastern State is the oldest public mental health facility in the country, operating since 1773. It is one of nine state-run facilities in Virginia, which collectively house 2,124 patients at a given time. Eastern State’s bed capacity usually numbers 302, but it was recently mandated to reduce that licensed capacity to 242 beds, operating at roughly 75% capacity despite an urgent need for bed space.
That capacity decrease order, issued by Commissioner of the DBHDS Allison Land, effectively halted new admissions to the hospital due to persistent staffing shortages. According to Assistant Director of Eastern State Dr. Dewey Jennings, without adequate staffing, the hospital cannot safely house its normal number of patients.
“The difference is with a hospital, any kind of hospital, you want to have a certain complement of staff to make sure you can safely take care of the patients and perform those duties,” Jennings said. “Based upon what was going on, I think the decision was made higher up to look at those situations and say, maybe we should start closing beds to make sure we’ve got adequate staff to take care of the patients.”
This decision to limit bed capacity made by Land, who did not respond to The Flat Hat’s request for comment, was not universally supported.
Virginia State Senator Montgomery Mason ’89, D-Williamsburg, is a founding member of the Joint Subcommittee to Study Mental Health Services in the commonwealth in the 21st century and considers Virginia’s mental health policy among his top priorities. He said that the decision to limit admission at the five facilities was unexpected and unwarranted.
“As far as how the decision was made to stop taking admissions, it was unilaterally done by the commissioner,” Mason said. “While I understand the concern of safety, we had had like 90 employees resign within a month period, we’d had 50-60 injuries. You know, you were just putting people in dangerous circumstances. I understand, but to unilaterally close down accepting patients was something that I just don’t know how she had the authority to do, right? But did.”
At a capacity of 242 patients, Eastern State can accept new admissions as other patients are discharged. However, a number of legal stipulations have limited admissions and kept the staff at Eastern State overwhelmed and the hospital in crisis mode.
The first stipulation involves the difference between civil and forensic admissions. Since Eastern State is a public facility, it must take on “forensic” cases — patients referred to psychiatric care by court order. These individuals are usually referred from jails and prisons, or they are found not guilty in criminal cases by reason of insanity. The high number of forensic patients waiting for admission to Eastern State has meant admissions for civil cases — any other patients coming from the community — have effectively ceased.
Just because Eastern State is admitting forensic cases does not mean it has the capacity to admit all of them — there is a waitlist. In 2015, the average wait time for incarcerated individuals in need of a bed at Eastern State was 73 days, according to The Washington Post. That figure was brought to light after Jamycheal Mitchell died in the Hampton Roads Regional Jail, where he was being held while waiting for a bed at Eastern State by orders from a judge. Mitchell was charged for stealing $5.00 worth of snacks from a 7-Eleven.
Additionally, Mason said not all individuals in forensic cases are in need of inpatient psychiatric care, such as that given at Eastern State. For example, individuals charged for misdemeanor offenses, like stealing or failure to appear in court, may not need inpatient status, yet still receive it. If not for charges pressed against them in the legal system, their conditions would likely be better treated by outpatient care, like therapy.
“55 to 60% of Eastern State’s admissions are forensic,” Mason said. “35 to 40% of those are from misdemeanor crimes. They are being sent to Eastern State because they're incompetent to stand trial for the restoration so they can come back and stand trial. For a misdemeanor crime.”
Mason said this trend occurs largely because law enforcement and court officials are not adequately trained to respond to low-grade crimes involving individuals with mental health complications. Currently, Williamsburg police officers undergo 40 hours of crisis intervention team training, which Director of Colonial Behavioral Health David Coe said isn’t perfect, but effective in increasing capacity and confidence of officers.
This training, however, is not required for officers prior to being hired — so not all active officers are trained. A community member would have to know this training exists in order to request a trained officer respond to their call.
Public hospitals thus bear the burden of all forensic cases, since court orders do not allow individuals to seek alternative care in private facilities. Mason spoke on distinguishing clearer requirements for admittance at public institutions such as Eastern State and pursuing alternative community-based programs.
“So part of this is up front trying to determine how we can divert from state hospitals,” Mason said. “But here's the thing not to be lost — while getting the person the treatment they actually need, right? It's not just about opening up, freeing up a bed. It's about properly treating. And that's where the stresses and pressures on our community based programs, run by the CSB, come into play.”
Community service boards, or CSBs, are the 41 state-sponsored organizations responsible for establishing and providing behavioral and psychiatric health services within their respective jurisdiction. Each board is led by an appointed board of directors which holds responsibility for providing adult and pediatric services for substance abuse, developmental disability and psychiatric health issues. Williamsburg lies under the jurisdiction of Colonial Behavioral Health led by Coe.

The second legal factor contributing to overcrowding in Virginia’s public mental health facilities is the 2014 “bed of last resort” law, which was spearheaded by Sen. Creigh Deeds, D-Bath. The law requires state psychiatric hospitals to admit patients under temporary detention orders if a bed cannot be found at another facility. TDOs are issued when a magistrate believes a person to be a harm to themselves or others, but they are unwilling to seek medical treatment on their own. Under a TDO, a person can be detained for 72 hours by law enforcement for emergency care before a civil hearing is conducted to determine whether that individual should be involuntarily committed to a psychiatric hospital.
Around the same time as the passing of the “last resort” law, Deeds also created the Deeds Commission, the precursor to the joint subcommittee on mental health, which has continued its work in the state legislature through 2021.
Deeds said the law was intended to ensure anyone is guaranteed treatment in a crisis. His push for the bill came after a tragic incident in late 2013, in which Deeds was stabbed by his son Gus, a student at the College of William and Mary who then died by suicide. A judge had ordered an involuntary temporary detention for Deeds’ son in the days leading up to the incident, though no hospital beds were available. The last resort law thus sought to avoid similar situations, and Deeds said it is still good policy.
“That bed of last resort legislation was designed to prevent a problem that was occurring in Virginia,” Deeds said “A number of times it occurred, people that had been taken before magistrates and evaluated by qualified personnel and found to be a danger to themselves or others. But they were released. They were put on the street because there wasn't room for them. They couldn't find a bed for them. Well, that's just that's bad policy.”
Though on paper, the law met its goal of mandating beds for all those in need, Interim Clinical Director at Eastern State Steve O’Brien said it has backfired in a sense, causing TDO admissions at public hospitals to rise from 3.7 cases a day in 2013 to over 18 per day in 2021, an over 500% increase that has overwhelmed facilities like Eastern State.
“I think it was probably effective in achieving that goal under the current statutes and laws and codes,” O’Brien said. “But the other effect was greatly increased our admissions and census. And you can look back at 2014 as the time when a lot of those strains started happening in state hospitals.”
Additionally, even though private and public hospitals have the same civil commitment laws and treatment processes, private hospitals can turn away patients if their conditions are deemed too severe, whereas public facilities like Eastern State cannot.
“As far as psychiatric conditions, we have no exclusionary criteria,” O’Brien said. “And so we will get people that none of the other hospitals will treat. So naturally, we end up with people who are more aggressive. Aggression is generally an exclusionary criteria for, say, a private psychiatric hospital.”
As a result, instances of violence against staff are especially prevalent in public facilities. In the 10-day period between July 1 and July 9, just before the capacity reduction announcement, there were 63 serious injuries among both the patients and staff within these facilities, which could range from fractures, eye injuries and permanent disability.
With fewer staff, those who remain at Eastern State face increasingly unsafe working conditions. In July, daily incidents or injuries to employees at facilities statewide were reported to average 4.5 per day. At Eastern State, “code” situations — crisis incidents or emergencies — happen often.
“It could happen daily, or it could happen every couple of days, or you could have a multiple in a day then go a few days, but it's common enough that, yes, it's happening,” O’Brien said. “You know, more often on a day than not.”
To mitigate difficult situations without resorting to physical force, Eastern State formed a crisis prevention response team last year. The team consists of a group of professionals trained in verbal de-escalation.
“Their sole job is to meet with the population, move through the population and help people that are having a really rough day,” Jennings said. “And we think it's been very successful. To the point that we believe it's led to some decreases in code situations here at the hospital.”
Ideally, O’Brien said, private hospitals should be handling 100% of civil admissions, whereas state-run hospitals would handle forensic cases and patients in need of long-term care, rather than patients who are not acutely ill. In the past, he said, private hospitals have acted as a funnel, taking all admissions and transferring patients in need of longer term care to state facilities. This arrangement is no longer the case.
Instead, hospitals often continue to house patients even after they are approved for discharge, since there are not adequate community resources to ensure their continued care. Patients who experience difficulties upon release, such as homelessness, are placed on extraordinary barriers lists. Until these patients are able to find placement in a local group home or other community-based solution, they stay at the hospital, potentially for years.
However, Vice President of Communications for the Virginia Hospital and Healthcare Association, VHHA, Julian Walker noted private hospitals are consistently handling a majority of both voluntary and involuntary psychiatric patients. VHHA is an organization that represents 110 private hospitals across the state.
“Those hospitals continue to handle all of the vast majority of total behavioral health inpatient hospital admissions across the board,” Walker said. “And you can break that down, or sort of separate that by category ... So our members handle all of the voluntary admissions in the commonwealth. Our members also continue to year over year handle the vast majority of the involuntary commitments.”
While Eastern State had to increase its operations to treat the influx in patients, it was not funded proportionately. With state funding trending downward for inpatient public mental health hospitals, Jennings and O’Brien said Eastern State has struggled to be competitive in recruiting staff. A nationwide shortage of healthcare workers has worsened the situation in an already-difficult sector. In order for Eastern State to increase bed capacity back to its normal level, Jennings said it needs more funding from the state to up the pay scale for direct care staff — staff that work face-to-face with patients.
Currently, the average salary at Eastern State is $55,714.14, a figure that includes the highest paid individuals. The highest paid staff are physicians, with a salary of $288,337. On the other end of the spectrum, food service technicians are paid as little as $20,748 a year, or $9.98 an hour. But more funding won’t come until next year’s state budget at the earliest, which will not be up for approval until July 1.
Some members of Congress have recommended limited redirecting of funding to establish community resources. Press secretary for Rep. Rob Wittman (VA-01) Sarah Newsome pointed to Wittman’s proposal to use remaining COVID-19 relief funds for the establishment of a crisis receiving center as an alternative to hospitalization. Wittman represents the congressional district in which Eastern State lies.
“I am happy to express my enthusiastic support for the establishment of a Crisis Receiving and Stabilization Center in Prince William County to provide much-needed access to mental health services to the over half-a-million residents of Prince William County and surrounding areas,” Wittman wrote in a letter to the chairman of the House Appropriations Committee Virginia House of Delegates. “The establishment of this Center reduces the dependency on the stressed hospital system. Furthermore, it reduces the impact on public safety officers and staff.”
During his time in office, Wittman has often voted against increasing funding for healthcare resources. Recently, he voted down a 2019 bill calling for workplace protection for healthcare workers, and in 2013, he co-sponsored a bill to repeal the Affordable Care Act.
In the long-term, Jennings and O’Brien said a shift toward community mental health care would prevent reliance on state institutions in general.
“The state of Virginia is going to have to make some decisions about how to expand the capacity of our mental health system,” O’Brien said. “It's time. And lawmakers are going to see that, and we really see some support over the next several years. You know, there's a lot of plans that have been put into place that are moving forward right now. And those need to continue to come to fruition, as well as a continued expansion, so we don't have the reliance on state institutions.”
For Deeds, revamping the state’s psychiatric care will require both increased support of existing programs, such as System Transformation Excellence and Performance VA, and the expansion of community-based services. STEP is a plan that was created by DBHDS in 2017 with the aim of increasing accessibility to mental health services, improving support to Virginia’s CSBs and providing patients with an array of resources.
The plan was to initially provide $8.9 million in funding from Virginia’s General fund dollars and Terry McAuliffe’s Governor’s Access Plan. However, the full expansion of the program has yet to occur, an issue which the program’s website attributes to inconsistent support and unstable funding.
Deeds also highlighted the need for investment in CSBs.
“It seems to me that the most efficient money we can spend, and it's going to take money upfront, the most efficient money we can spend is to dramatically rebuild our CSBs, invest in people that work there,” Deeds said. “Make sure those jobs are rewarding. Make sure we have enough people in every CSB in Virginia. And, you know, keep people out of crisis and keep them out of hospitals.”
Coe said CSBs, like hospitals, are in crisis. Instead of referring to the system as broken, Coe said it was incomplete due to underfunding.
“That's real simple,” Coe said. “The answer is no, the funding is not adequate. Virginia is pretty famous for not funding things adequately. I would hope they would do this one differently. I'm not optimistic … I've been doing this work for 31 years, and 31 years has not given me reason to be optimistic.”
Along with the need for immediate fixes, policymakers and community advocates are calling for implementation of longer-term solutions. These include alternative care options, new government programs and an increase in community based treatment.
Mason said state action on mental health has historically been reactionary, such as policy implementation following the mass shooting at the Virginia Tech in 2007 and similar changes after the Deeds incident. Mason views the subcommittee on mental health as a way to ensure sustained action.
“It's an effort to make it an ongoing, continual conversation that we have, in order to face the challenges we need to address and try to make the system better,” Mason said. “And we're always going to have challenges, always going to be resource constrained, but we can't just address it through tragedy.”
Mental health initiatives inevitably compete with other budget priorities, meaning they often receive less funding than their proponents request.
“The budget is a negotiation of all, this is just one element of it,” Mason said. “It's a negotiation of all that funding … I could come up with 10 places that are going to come in and request that and show a noted need that they need 250 million dollars.”
Mason specified the bolstering of the few Crisis Intervention Team Assessment Centers, or CITACs, as a possible solution to overcrowding in hospitals, and has pushed for the eventual implementation of additional CITAC programs across the state. CITACs operated under the jurisdiction of the local community service board. Mason hopes these programs will be instrumental in redefining Virginia's mental health care system.
Already operating at various public and private hospitals and health centers in Virginia, CITAC programs provide alternative assessment and support options for mental health crises that may have been previously handled solely by law enforcement. With CITACs, officers who identify individuals they believe are struggling with mental illness can direct them to healthcare professionals. In Williamsburg, Riverside Doctors Hospital’s emergency unit has a CITAC team that operates from midnight to noon.
Coe said the CITAC unit has reduced the burden of handling crisis cases for Colonial Behavioral Health.
“And it really has allowed law enforcement to not have to spend so many hours sitting and waiting, you know, with folks in the emergency room while they're in custody,” Coe said. “So that has been utilized by all four of our localities.”
Additionally, a new emergency number, 988, has been established nationwide in a similar attempt to divert mental health crises away from the police. If called, a local representative will provide resources under three designations: trained staff members to speak with, dispatch of a mobile crisis team and/or crisis stabilization programs that consist of short-term observation such as hospitalization. Williamsburg does not currently have a mobile crisis team, which are designed to respond to 988 calls, but Coe says Colonial Behavioral Health intends to have a team up and running within the next year.
Though Mason emphasized urgency surrounding mental health reform, he said budget negotiations are a barrier to adequate funding. According to Mason, in response to the Behavioral Health Commission's request for $37 million to expand these programs and similar efforts, they were provided just $10.5 million. Deeds echoed the difficulties in funding community mental health resources.
“If you look at the maps, every Virginia locality, basically, is a medically underserved area in the niche area of behavioral health, and the needs are so dramatic,” Deeds said.
“If you look at the maps, every Virginia locality, basically, is a medically underserved area in the niche area of behavioral health, and the needs are so dramatic,” Deeds said.
An upcoming project in Williamsburg called Hope Family Village adopts a radically integrated view of community mental health care to address this deficit. The village is essentially a neighborhood, situated on 25 acres of Eastern State surplus land, where people with mental health conditions can live with their families and care for one another. Vice President and Director of Hope Family Village Lisa Randolph said the project is the brainchild of a family support group run by the National Alliance of Mental Illness’s Williamsburg chapter, which began developing the idea in April 2014.
“There was a very common theme that came up over and over again in the support group and that was having our loved ones live in a community of caring and acceptance, a place that was safe,” Randolph said.
Many in the group, including Randolph, had loved ones hospitalized in the past. The idea behind the village is to avoid the need for inpatient care altogether.
“The state is at an all time crisis and Eastern State has such a staffing shortage that they've actually reduced the number of beds that are available,” Randolph said. “So we started thinking about what a community might look like and at the same time, we also discovered something called cohousing.”
Cohousing is a setup in which residents live in private homes clustered around public spaces, where they share meals, collectively care for the neighborhood and engage in shared activities. Randolph said Hope Family Village is the first cohousing community dedicated to mental health in the country. Though Randolph acknowledged that the village is small scale — it will house just 25 families — she views it as a model for similar communities across the country.
“Our plan is to be a model community,” Randolph said. “Then as we're writing grants, a lot of times you can find innovation funding for new models. So our goal is to sort of pitch this as an innovative model and to use our little Hope Family Village in Williamsburg as an experiment, as a grand experiment. And start to document some results and to prove that the concept works. As a kind of proof of concept.”
With a new governor preparing to start his time in office, Virginia’s mental health care systems continue to face uncertainty. For Coe, the entire system needs to be reimagined.
“Before, the system was built upon the idea that communities would be your core care model, and the safety net for the community was the hospital and people in the hospital system,” Coe said. “From a systems perspective, what I've seen occur is that the community has now become the safety net for the state. That's weird. But it's where we are.”